Both structural and technological challenges mean that community-based health and social care providers' face an uphill battle as they work to improve the wellbeing of our most vulnerable.
Noted was founded in 2015 to realise ideas I had to capture pragmatic outcomes in case notes in 2013. Since that time, we have been focussed on meeting the client management needs of community based health and social care providers in Aotearoa.
We started with allied health providers in small, private practices and have since moved on to provide services to the mental health teams of about 15% of New Zealand secondary schools; a range of social service providers; large mental health and counselling services; some of the largest Māori Health Providers in Aotearoa; and primary health organisations, the largest of which is Pegasus Health.

Over that time, I have had the privilege to work with many incredibly dedicated, talented people, whose main motivation is to increase the wellbeing of their whānau. I have also had the opportunity to understand the challenges they face and consider where the opportunities for improvement lie.
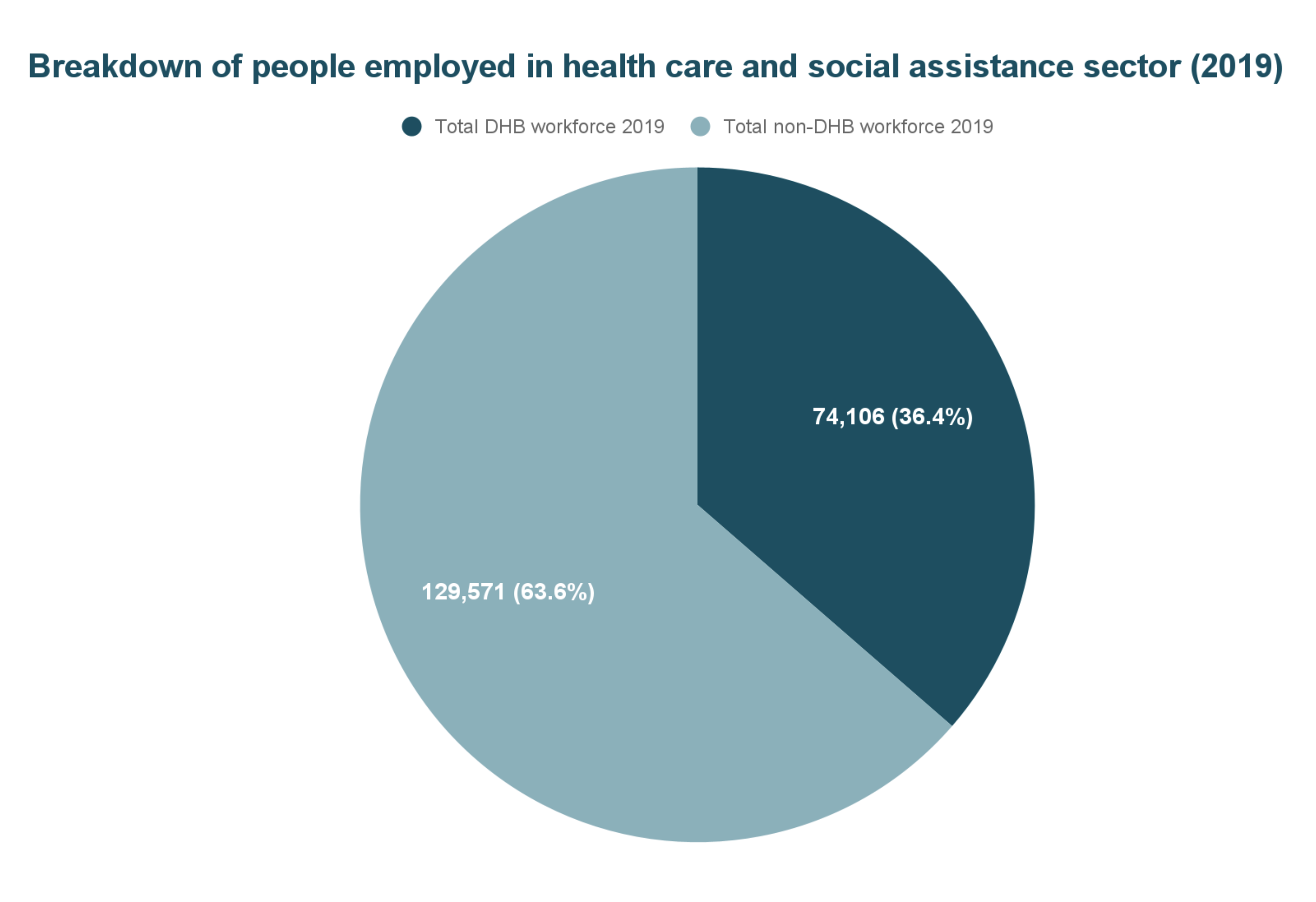
To put things into perspective, we are not talking about a small group. According to a 2020 report published by Manatū Hauora, 64% - about 130,000 - of health and disability workers, work outside of services provided by the old district health boards.
This was recently acknowledged in an April press release promoting Leigh Donoghue starting as Chief of Data and Digital and the Hira programme. To quote Fepulea’i Margie Apa, Chief Executive of Te Whatu Ora: “... most contact work is actually happening in communities”.
It is not a new idea that interventions in the community are more likely to improve the overall quality of life of our people, while also reducing the load on secondary care. Meanwhile, studies both overseas and in Aotearoa, have shown that working with whānau, rather than merely individuals, improves outcomes.
Given the importance of community-based care, it would seem intuitive that the community-based health and social sector would be well served with appropriately easy access to funding, and efficient systems to work from. We’d also expect providers to have access to the data they need to manage themselves and for the government to have access to extensive data on the needs of people, work undertaken and the impact of that work. Given the value of whānau-centric care, we’d expect this to also play an important role.
It will not be news to any of you, that none of this is currently true. The reasons for this are complex, and the answers are also complicated. While I do not claim to have a magic wand, I have some observations and experience to share, and it is my hope that some of this may prove useful at this time of rapid change.
First I’ll summarise my view of the status quo, then move onto possible solutions. Finally, I will share some of the approaches we have taken at Noted.
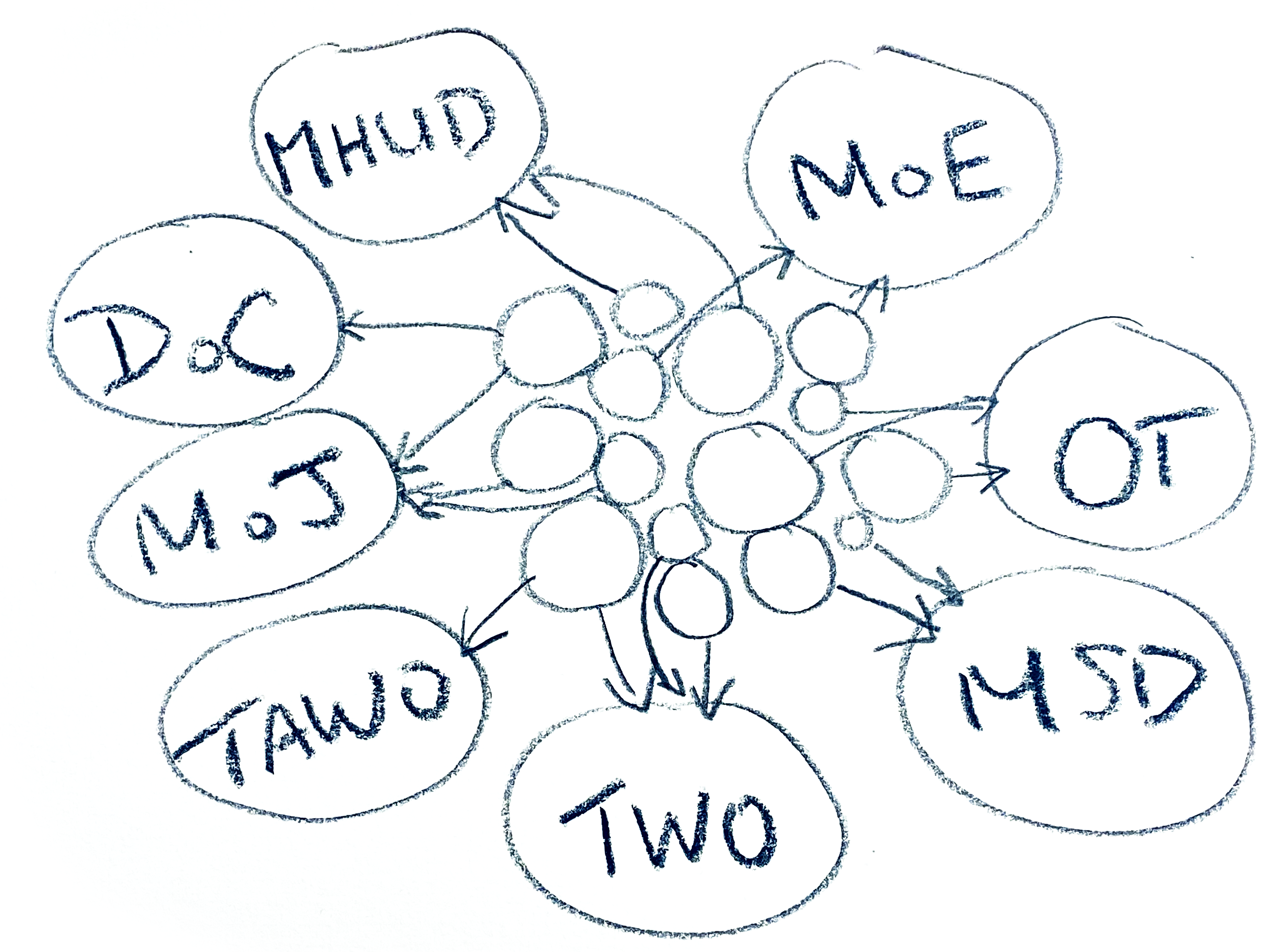
In this diagram, the circles in the middle represent teams in a community-based care provider, with the arrows representing data flows out to contract providers. This image isn’t actually nearly chaotic enough - a large Māori health provider could well have over 50 contracts to manage.
Important here, is that a lot of the stress imposed on care providers comes from the way they are funded.
Contracts are won from a range of government departments, or entities, with each one requiring its own unique set of data to be delivered.
The data required can seem pretty arbitrary to those who have to provide it, and these data can vary from region to region. This is inefficient, can leave staff questioning the value of the effort required, and makes creation of a national picture more difficult.
Constantly fighting to gain, and retain contracts, adds a high level of uncertainty, increases the stress levels of managers and executives, and makes planning hard.
This funding model also exacerbates the tendency towards siloed systems - especially when the contract requires use of an external system, provided by the funder.
This, in turn, leads to a lack of coordination between internal teams - let alone between agencies.
There is also an inevitable lack of access to useful datasets, and a lack of centralised data that a care provider can use. Information goes back to funders but is often not aggregated with data from other services the care provider delivers. Many organisations do not even know how many clients they have.
There is also a lack of systems built for the broad scope of community-based health and social services.
This often leads to staff working on systems that are not designed for their mahi, for example using medical PMS for mental health delivery.
Staff will often manually maintain spreadsheets alongside their case notes. This, in turn, can lead to compromised, or unreliable data quality.
As you will have figured out by now, I think a lot of the problems go back to how community-based organisations are funded. I think that a far better approach would be bulk funding for organisations to deliver on measurable outcomes.
I feel that a much more efficient funding alternative would be to provide organisations with the funding they need to operate, as a cohesive whole, to deliver on agreed outcomes. This would significantly reduce their administrative load and put the focus back on outcomes - not counting stuff.
It also acknowledges that health outcomes are inextricably linked with other influences, such as employment, education, income and housing.
An interesting complication here is that currently funding for one provider may well be coming from many government departments:
- Oranga Tamariki - Ministry for Children
- Te Manatū Whakahiato Ora - Ministry of Social Development
- Te Whatu Ora - Health New Zealand
- Te Aka Whai Ora - Māori Health Authority
- Te Tāhū o te Ture - Ministry of Justice
- Ara Poutama Aotearoa - Department of Corrections
- And so on
Maybe the answer is a centralised, pan-agency commissioning agency, beyond the scope of Whānau Ora?
From our experience, another step forward would be to have as many staff as possible working from a unified system. It is much easier to coordinate care if all information on a client is held in a single repository. It makes data collection easier, too.
For it to work, the system needs to be configured for each team, so they can work safely and efficiently, with an ideal workflow.
Sophisticated access controls are important if this is to work. With a lot of sensitive data held in a single location, it is critical that the information is filtered so that each user only sees what they should.
It also makes sense to capture as much queryable information as possible in the case notes of staff so data capture isn’t adding to their workload.
I believe that whānau should be a first class entity in the system. Conceptually, I believe that a whānau should be seen as a client in its own right, with its own history, goals, needs and outcomes.
Alongside this, integration between systems is mission critical. No one system can - or should - solve everything for everyone, and that is where the ability to connect with other systems comes in. Personally, I am excited about the work Hira is doing in this space, and the work already done by HealthOne.
To my mind, people and whānau-centric care is only possible if people and whānau can appropriately access their data, give and remove consent, and generally engage with their care providers via their own devices.
Data standards are also important. Data organised into well defined concepts that can be then aggregated appropriately with data from other organisations is the path to service providers delivering informed care and funders making properly informed spending decisions.
Finally, we think it would be awesome to create a centralised data warehouse - or series of centralised data warehouses - that store relevant data, that agencies can then query themselves to measure provider activity and holistic progress towards outcomes. In this scenario, data would be delivered programatically from providers’ systems and the analytics load would be carried by government agencies.
With all this in mind, I will take this opportunity to share how we have applied some of these concepts in Noted, already, and give a quick preview of what we are working towards.
In Noted, case notes are captured in context specific, dynamic structured forms that enable workers to transparently capture queryable data as they take their notes.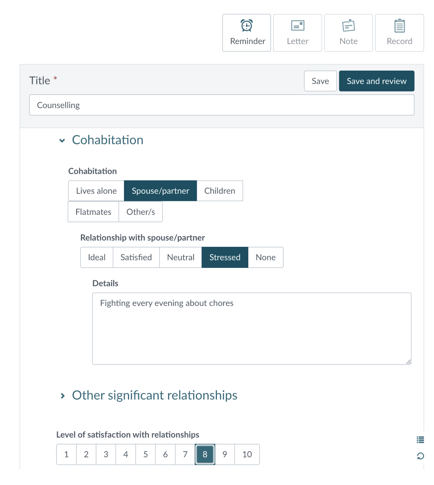
Semi-structured forms make it quick to enter information that can be reported on, while there are still lots of opportunities to capture the accompanying narrative. Risk assessments, and other form elements, appear as required.
Follow up records support staff to revisit key themes and, especially when it comes to numeric scales, the likelihood of capturing contiguous data is increased.
The forms have been shown to significantly increase the speed that notes can be written, while standardising workflow within teams.
Especially within the context of community-based care where one organisation could be delivering cancer screening, family violence, alcohol and other drugs addiction treatment, transitional housing, early childhood education, and budgeting support, it is critical that users of the system only see what is relevant to them.
Noted’s approach is non-hierarchical, which means that access is not predicated by whether a user is a manager or not - but rather by what they need to do their job.
By default, access controls are applied according to the team that is creating the record. 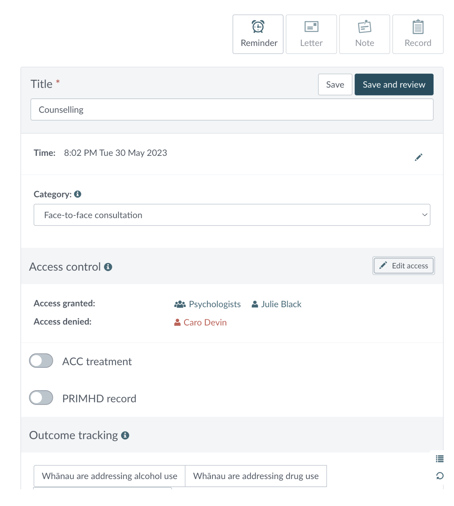
Additional fine-grained control is also given to access to:
- Individual records
- Individual clients
- Groups
- Whānau
- And various other entities in the system
Based on the requirements of customers, Noted was developed to provide 3 levels of access to records:
- Full access - every staff member can read the record
- Limited access - it is possible for all to see a record exists, and who wrote it, but not read it
- No access: it is possible to hide that a client has any interaction with a team at all
Role groups also provide easy control over who can access features and privileges in the system.
In Noted, a whānau is a ‘client made up of clients’. A client can be added to multiple whānau and the definition of a whānau is left to the business rules of the provider.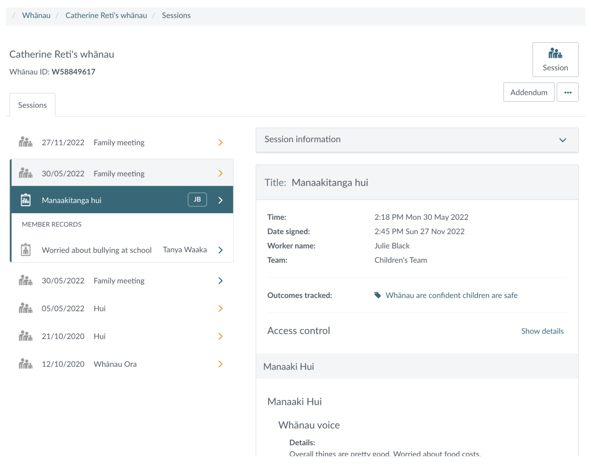
Interestingly, the whānau feature is not just used by Māori health providers, delivering on Whānau Ora contracts. It is also popular with other social service providers who work with whānau.
Records on sessions with whānau are kept in one place, and the case notes also flow through to the whānau members’ notes, so they can be read on the individual, or on the whānau with ease.
Fully integrating with other systems in the ecosystem is a work in progress. So far, we have integrations with ACC billing, PRIMHD and various school management systems.
As part of our partnership with Pegasus Health and other South Island customers, we have committed to integrating with ERMS and HealthOne.
Other roadmapped integrations include:
- Hira: Starting with identity management
- Medicly, which will allow us to access, utilise and aggregate data from New Zealand medical PMS systems
- We will also be integrating with systems that will enable Noted to send and receive messages and other information from other frontline systems, including those used in Primary and Secondary care
- Finally, We will be working to make data held in Noted available to other systems via a well documented, RESTful API
Capturing information, both quantitative and qualitative, is important, but this is of little value without the ability to access it.
Noted’s approach to solving this is to synchronise data from its application database to its own data warehouse, where the data is renormalised and surfaced to users in with a sophisticated series of apps in Qlik Cloud.
The tools enable non data analysts, such as frontline team leads, to access the information they need to:
- Manage their team’s data quality
- Manage worker caseload
- View their referral pipeline
- Analyse outcomes
- And access information for funders
In its entirety, we see Noted’s data discovery solution as providing community based care providers with the data analytics capabilities normally only available to very large organisations, such as hospitals.
Terms used are user defined, with a rich data dictionary providing a list of key concepts that can be labelled according to the terminology of the customer. An example would be the concept of ‘client’ which could equally be called ‘tangata’, ‘whaiora’ or ‘patient’. The concept remains constant.
Over 300 concepts have now been defined and work is continuing steadily.
This is important because it will enable data from multiple customers and systems to be aggregated and queried, without limiting the ability of customers to use the language of their choice for their own use.
Despite years of work, there is still much work to do. A couple of projects we are impatiently waiting to start work on, include:
- A client/whānau app for a small mobile device that will enable people to:
- Access their records
- Provide and remove consent
- Control who can access their records
- Message staff
- And make appointments
- We are also planning a sophisticated referral management system that will seamlessly send and receive referrals to or from other systems, while also providing our users with an awesome experience for managing the journey of whānau through our system.
In conclusion, currently, many community-based health and social care providers tend to be working on siloed systems that don’t support the diversity and sensitivity of their work and they spend far too much time trying to meet the requirements of funders.
I believe that many of the issues faced by community-based providers go back to how they are funded, with many contracts, and constant uncertainty for managers.
Organisations need to be able to work efficiently from a unified system, that is connected with the wider ecosystem, while capturing the information they need to inform care and funding decisions. This includes the ability to work with whānau as entities in their own right.
With the degree of change that is currently in progress, I believe that we have a once in a generation opportunity to develop a completely new approach to how we support the wellbeing of the people of Aotearoa.
Noted is excited at the prospect of being part of the solution.
About Noted
Noted is a people and whānau-centred client management system that empowers health and social care providers to care for their whānau from a unified platform, with unparalleled access to data insights.
Based in Wellington, Noted Limited was founded by Scott Pearson in October 2015, and has customers that include primary and secondary care organisations, Māori health providers, social service providers and mental health providers, including over 10% of Aotearoa's secondary school hauora teams.
Contact details
Scott Pearson
Founder | Chief Strategy Officer
+64 21 634 567