Introduction
Last year I spoke about the challenges faced by community-based health and social care providers, delivering to many funders, across multiple government entities.
To summarise, I talked about how community-based providers often have many, diverse teams, working on disparate, disconnected, and often substandard systems that impair their ability to coordinate the delivery of care, attain an organisation-wide view of their whānau, and the impact of their mahi. I also discussed how this situation has been brought about, in part, by the way the sector is funded.
Over the last 12 months I feel I have gained a better understanding of the wider ecosystem and now appreciate that the challenges I identified are by no means limited to community-based providers. The issues discussed are also relevant within government organisations, including Health New Zealand.
In this piece, I am going to zoom right out and share some further thoughts on how services are funded, the value of capturing the impact of wellbeing created by services, and concepts and technology that Noted is pioneering that enable the implementation of the ideas.
Our health and social sectors are under extreme pressure. Both from a financial and workforce perspective, we all need to do more with less. Governments, providers and staff alike need to know they are getting the best return possible - whether it is for taxpayers’ dollars, or their blood, sweat and tears.
“Governments, providers and staff alike need to know they are getting the best return possible - whether it is for taxpayers’ dollars, or their blood, sweat and tears.”
We need a system shift; to move away from funding just to deliver a particular service and instead funding to improve the wellbeing of people. If we can measure the impact of services on wellbeing, then we can determine where to allocate scarce resources to have the most impact.
I see the path to this as capturing data at the frontline that allows us to understand the wellbeing of people as they move through our care, and then aggregating these data to get a population view.

Capture the right information
For many contracts, funder reporting is about counting stuff. How many contacts; how many things provided; how many kilometres travelled.
From the point of view of a provider demonstrating they have done something for their funding, this makes sense, but it offers no insight into the impact of the work done.
A solution to this has been to track indicators. This requires recording whether certain factors are present or not, with the assumption that these factors are an analogue for wellbeing. To give an overly simplified example, a house may have a kitchen, bathroom and 3 bedrooms “tick!” but if it is mouldy then it isn’t necessarily going to be a positive influence on its inhabitants wellbeing. This measure is also unlikely to capture the voice of the people who live in the house.
“Maybe the question that drives funders should not be, ‘What did they do?’, but rather, ‘What did they do to achieve that change in wellbeing?’”
A third option is to track wellbeing aspects. In this case, frontline staff, and people receiving care, are giving their score on a particular area of their wellbeing. This allows for a much more nuanced response, as the score can take in all the information available, rather than being limited to a predefined subset that may not answer the underlying question.
It will come as no surprise that I’m proposing capturing wellbeing aspects is vastly superior to the first two options.
Does this mean that I am suggesting that we omit counting stuff? Actually, no. We still need to capture our activity, but maybe look at it from a different perspective. Maybe the question that drives funders should not be, ‘What did they do?’, but rather, ‘What did they do to achieve that change in wellbeing?’
Aggregate data
The information captured by a provider becomes much more useful when it is aggregated with information from across the sector. For this, data classifications such as HISO and SNOMED, in conjunction with HL7 FHIR, are critical; but as their main focus is on primary and secondary care, the existing standards are not currently broad enough in scope.
The main suggestion I have on this subject is that the classifications be extended to include wellbeing aspects, to support a shift in focus towards capturing and measuring wellbeing impact. With that said, creating standards is only really useful if the systems staff use make it practical to capture and collate required data.

Systems that are fit for purpose
Delivering on the needs of staff, health and social provider organisations, and government agencies requires systems that provide end-to-end data capture and analysis that are easy to use, efficient and, so far as possible, automated.
Work has already begun on the National Data Platform which offers the required centralised repository, but how will conformant data be captured? And how will it arrive in the NDP without compromising the needs of those who created it in the first place?
At Noted, in conjunction with various complex health and social care providers, in particular Māori health providers, we have been working hard to solve many aspects of this puzzle, including seamless data capture with our own library of data domains, automatically synchronising with our data discovery solution. Using our event driven architecture, certain data could be automatically delivered to the NDP.
Noted has taken a platform approach, with a single codebase and standardised tools that make the system highly scalable, and is committed to integrating as seamlessly as possible with the wider health and social ecosystem.
Seamless data capture from case notes
Noted is built on the idea of making it easier to take case notes that contain useful, queryable data, using context specific, dynamic structure forms. The forms are highly malleable, meaning that they can be easily tailored to the requirements of individual teams, while also capturing standardised data.
Data domains
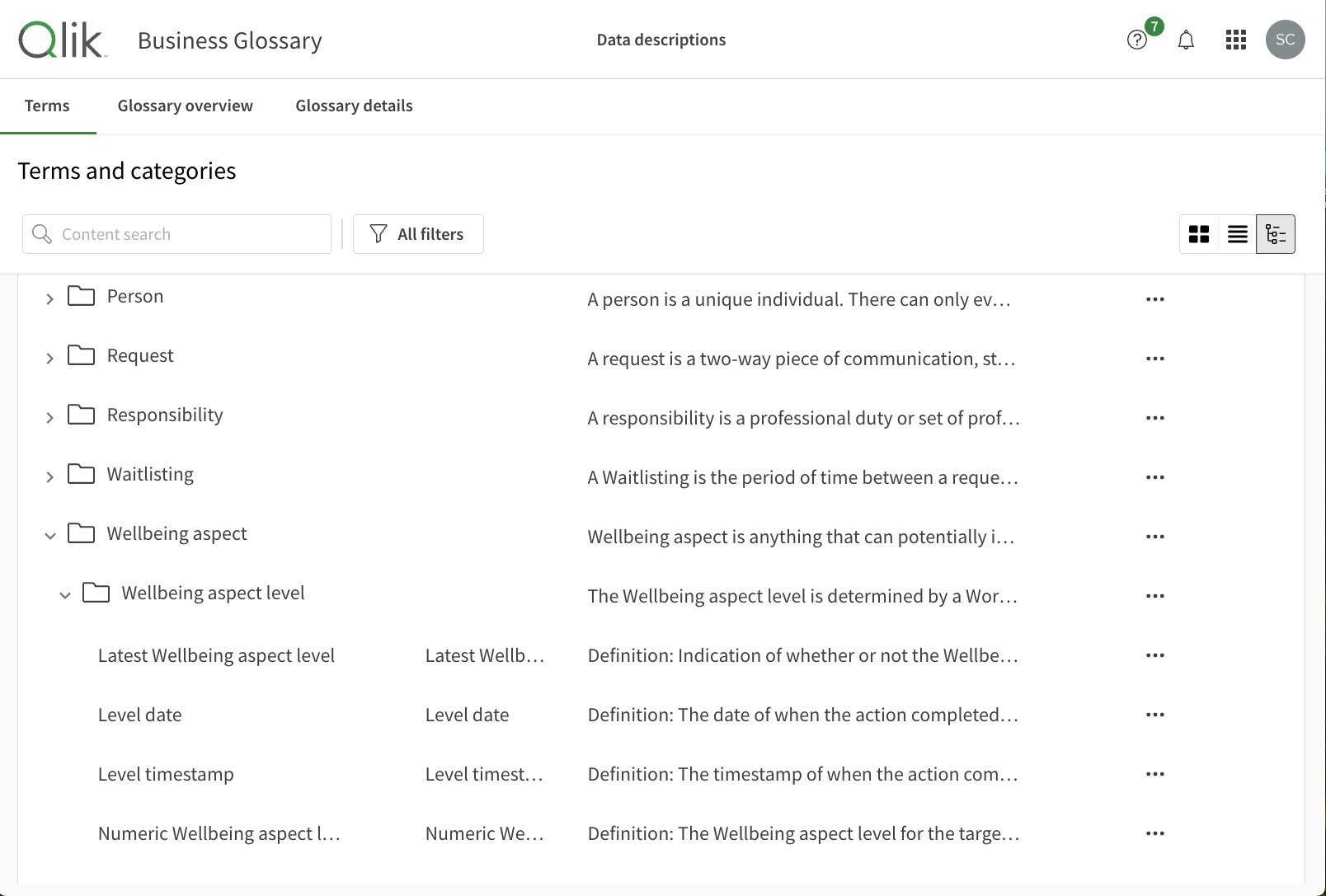
For over two years, we have been continually developing a library of data domains for everything from whānau, to whakapapa, to wellbeing aspects. This mahi has been led by our data architect Dr. Pernille Christensen, working in close collaboration with Rachel Henare, our Chief Customer Officer, the rest of our customer team, and our customers.
For the most part, the domains do not overlap with existing HISO standards, or other data classifications, as we have focussed on community-based care and areas not yet classified.
Our data domains are built into standardised code used to create our forms and are even starting to inform the language used in the application itself.
Data Discovery
Using our ETL process, data are automatically synchronised through to each customer’s data mart and then surfaced to them with a rich collection of standardised data discovery tools built in Qlik Cloud.
There are a number of advantages to this standardised data approach:
-
- It is easy to onboard new customers
- Data captured by a provider during work on a plethora of contracts can be aggregated and analysed according to need
- Data from different providers can equally be aggregated and analysed using the same data discovery tools, with certain data being pulled into new locations for specific purposes
- This is powerful solution for funders, solving the many issues associated with receiving and ingesting data from multiple sourceWe expect to be offering a similar service to share data with the NDP
- We expect to be offering a similar service to share data with the NDP
Platform approach
The standardised approach discussed also applies to the client management system itself.
Noted is a single codebase. Its combination of sophisticated access controls and easy configuration of organisations and teams means that all users are working with a system that is tailored specifically to their needs, while still working on the same system.
Noted’s data discovery solution means that an organisation can maintain data sovereignty over, and access and manage, the data of all of its services and population.
With the implementation of data discovery for contract providers, such as Health New Zealand, contract specific data can be appropriately shared from multiple vendors.
In parallel, Noted could also be sharing relevant data with the National Data Platform.
Integrations
Noted is only a small part of the wider ecosystem and it needs to be as integrated as possible. With our partnership with Medicly, we already offer data ingestion from GP practice management systems, with the option to surface certain data within the Noted app and/or Data Discovery.
In cases where funders have providers not using Noted, but want to use our data discovery tools, data could be ingested into Noted using a similar method.
Noted is committed to integrating with services from Health New Zealand, and systems from other relevant organisations.
Conclusion

With such limited resources available to it, the government needs to be able to understand the impact of its investments on our wellbeing.
To enable this, wellbeing information needs to be captured seamlessly during the everyday work of frontline staff and then aggregated to provide a population view.
This needs to be implemented without creating silos within providers and with as much automation as possible.
By developing a rich library of data domains and standardised data discovery tools, and leveraging the benefits of its highly configurable client management platform, I believe that Noted has come a long way to solving the challenges faced.






